Ona Daugirdas.
During this uncertain time caused by the coronavirus pandemic, every one of us is concerned with our own safety. We are re-organizing our lives, shielding ourselves from the potentially sick to avoid infection. It is easy to forget that this strategy is not an option for medical personnel, who jeopardize their health every day while caring for the sick.
New York City is currently the epicenter of the coronavirus pandemic in the U.S. The city’s hospitals are overwhelmed by thousands of patients and are facing critical shortages of medical supplies. Among the medical staff working on the front lines of this pandemic in NYC is a young Lithuanian American doctor, Vytas Vaitkus. He is Board Certified in Internal Medicine and Pulmonary Disease and completing his training in Critical Care Medicine. I recently spoke with him by phone at 4 o’clock in the afternoon, waking the sleep-deprived doctor from an already too short a rest. When I apologized, Dr. Vaitkus graciously replied that he had to get up anyway and get ready to work the night shift. We spoke about his work treating New York’s Covid-19 patients.
Dr. Vaitkus, tell us a bit about yourself and how you came to be in New York, confronting the ongoing pandemic.
I was born and raised in Cleveland. After graduating from Ohio University with a degree in medicine, I came to New York for my Internal Medicine residency. Subsequently, I completed an additional year as Chief Resident and am now specializing in Pulmonary Disease and Critical Care Medicine. I have now lived in New York for seven years. Just as the whole world is today, I am experiencing unimaginable events, perhaps only on a different level.
Is there a shortage of doctors and medical staff?
Let me answer the question indirectly. Several weeks ago, on a Saturday, I examined a patient. The following Monday, I was informed that the patient was positive for the Covid-19. I was directed to stay at home and self-quarantine for 14 days. After only two days of quarantine, I was summoned back to work and told to wear an N-95 mask and monitor myself for symptoms. Apparently, the hospital administration realized that if it adhered to the official self-quarantine guidelines, soon there wouldn’t be enough doctors or other personnel left at the hospital. So I worked while potentially being infected, and the patient risked being cared for by a doctor who had been exposed. I currently work 12-hour shifts, six days in a row, then I get one day off, and the cycle starts again. Decide for yourself whether there are enough doctors.
In your estimation, what percentage of patients in the hospital are infected with the coronavirus?
Until a few weeks ago, we had two categories of patients ‒ those infected with the virus and those in the hospital for other reasons. Currently, coronavirus patients occupy all of the beds. In our program, we are a total of 20 Pulmonary Fellows (specialists) who rotate through five New York hospitals. This includes Kings County Hospital, a large public city hospital (comparable to Chicago’s Cook County Hospital, only twice as large). My most recent appointment is to SUNY Downstate Hospital, which is now designated exclusively as a corona hospital. You can just imagine how difficult it is for the staff to work day-to-day in a hospital completely full of Covid-19 patients and concurrently try to protect themselves from infection.

What about the issue of personal protection? Currently, the situation appears to be improving, but how did you deal with the lack of gloves, masks, and gowns?
For a long time, I would arrive at work, never knowing if the hospital could provide the needed supplies that day. I will admit, I did some hard soul-searching about what I would do if I were asked to work without protection. Would I be willing to risk my own life to provide life-saving care to someone else? It was a tough thing to consider. But thankfully, it never came to that. Somehow miraculously, the needed supplies would materialize. Guards were stationed at the hospital stockrooms, making sure no one took anything without permission. Elsewhere, protective equipment was actually locked up in narcotics cabinets ‒ the most secure places in the hospital.
All the supplies were extremely carefully rationed. At the beginning of the crisis, a tent was set up outside of the hospital for coronavirus diagnostic tests. Gloves and masks had to be changed after each patient, resulting in vast amounts of protective equipment being used up every day. Given the dire shortages in the hospital itself, the service became unsustainable, and the diagnostic tent was quickly shut down. Here’s another example. Two doctors from another department were sent to help our Intensive Care Unit (ICU) staff. However, they were not allowed to equip themselves with protective gear from our ICU supply. These good Samaritans were told they had to furnish their own equipment from somewhere else.
We should call you a Corona warrior. How do you dress for work?
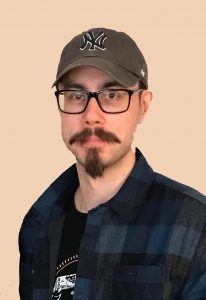
First, I put on surgical scrubs. Over that, I put on paper scrubs. Since the tops of both scrubs have short sleeves, I put on a third layer, a surgical gown with long sleeves. Next, I put on an N-95 mask. This mask is designed to be re-used multiple times, so on top of it, I place a single-use face mask. And since the eyes and the upper part of the face still need to be protected (glasses offer no protection), a transparent surgical shield is worn over everything. And, of course, I wear gloves and shoe coverings. Part of this outfit must be changed after examining each patient. Additionally, I had to shave off my mustache and beard so that the mask would fit snugly against the skin.

Now that every single patient in my current hospital is infected with the coronavirus, the attire has become somewhat simpler. There is no need to protect the uninfected – there are none! As you can see in the photo, I now only wear overalls over my scrubs. After I examine the patients, I don’t need to change the gowns anymore. My parents from Cleveland provided me with a high-quality 3M 6800 respirator helmet with a very effective P-100 filter. It doesn’t heat up and allows easy breathing while wearing it. All of my colleagues are envious.
Can you comment on the shortage of ventilators?
Yes, there is a lack of equipment, but that is just the tip of the iceberg. Even if there were millions of ventilators available today, hospitals would need more ICU units to place them in. And you would need specially trained staff to manage them. Otherwise, this precious commodity will have to languish in hospital basements and factory warehouses. Ventilated patients currently occupy all the beds in our Medical ICU. Because elective surgeries are no longer performed, the entire Surgical ICU has been given over to corona patients. Even the Pediatric ICU has been commandeered ‒ it has raised its admission age limit to 30 years in order to accommodate young adults.
Doctors in the Emergency Room have ingeniously constructed temporary breathing aids for their patients when they did not have ventilators available. Using gauze to tightly mount a CPAP mask (usually used for sleep apnea) on the patient’s face, the doctors hooked up spare ventilator tubes, inserted a valve, and connected everything directly to a supply of wall oxygen. There is no way to check the air pressure or the amount of oxygen delivered, but what do you do when the patient is short of breath and hypoxic, and there is no other option? Thanks to their creativity, these doctors have saved many lives. Such conditions must only exist on a battlefield.

Of your patients in the Intensive Care Unit, how many of them have improved enough to be transferred out?
One.
Sounds like being put in the ICU is equivalent to a death sentence…
Essentially.
After a patient dies in the hospital, what then?
Our hospital morgue is full. As a result, a body often has to remain on the ward until a place in the morgue opens up. The unpleasant reality is that there is simply nowhere to put the deceased.
Why is there such a high Covid-19 mortality rate?
For one thing, the course of the disease is insidious. E.R. doctors, after examining patients with possible signs of Covid-19, maybe even with some X-ray evidence of pneumonia, but without shortness of breath, have no choice but to send them home to rest and recover. There is a significant risk in hospitalizing infected but stable patients, and hospitals simply don’t have room. Unfortunately, after several days, some of these same patients return in critical condition with overwhelming respiratory distress. The virus appears to cause a very powerful inflammatory reaction in the lungs and elsewhere, which triggers a cascade of other complications. And treating one complication inevitably leads to other devastating problems.

Furthermore, we do not have any effective medicine to treat Covid-19 at this time. In caring for these extremely critically ill patients, we have judiciously tried many treatments. At first, some medications seem to improve the patient’s condition, and we become hopeful, but each time, the effects prove temporary, and the patient deteriorates again. Mortality risk also is dependent on the person’s entire health profile. If there is heart or lung disease, high blood pressure, diabetes, or the patient is elderly, the risk of dying increases significantly. In addition, the size of the population at risk is enormous ‒ the novel coronavirus is a new variant of an old virus. Not enough of us have contracted it to confer herd immunity and make the world less susceptible. So bottom line, we are all at risk.
Why do you think the virus has spread so wildly in New York City?
I believe several factors are at play. NYC is a very large city with high population density and a lot of poverty, which makes it conducive to disease spread. But having said that, a significant factor is irresponsible behavior. The governor was initially hesitant to enact restrictions, and our mayor, in contrast with those of other large U.S. cities, was in no hurry to close schools, businesses, or restrict the movement of people. Neither did he apply the rules to himself ‒ he was photographed leaving his gym club during the restriction. Where was his good example?
And the people of the city, especially the young crowd, simply ignored warnings and instructions. On my way to work, I often saw large groups clustering on the sidewalks, near restaurants, and in the parks. Despite the barrage of news about New York being in a major pandemic crisis and constant reminders for people to stay home, I saw photos of crowds of people gathered to see the USNS Comfort hospital ship sailing into New York Harbor. Is it really so important to take that forgettable selfie, risk your health (by selfish choice), and then expect hospitals and medical personnel (who don’t have the option) to risk their lives to save yours? No, that photo is totally not important. But they are not thinking…
April 2

We have exchanged the latest information with Dr. Vytas Vaitkus. He said that while everyone is still talking about a lack of ventilators, a more significant deficit is beginning to emerge. Intensive care units are faced with shortages of essential medications, such as those used by doctors during intubation. This medication is also used to sedate patients on ventilators and prevent them from pulling out the ventilation tubing. Another hospital reported that they are facing a shortage of vasopressor drugs that raise blood pressure in cases of critical hypotension. Other medications are also becoming in short supply. Additionally, patients are dying at an increasing rate with rapid progression from respiratory to kidney and heart failure. Dr. Vaitkus described the admission of patients as having become a game of checkers ‒ an attempt to shuffle beds for new admissions, the critically ill, and the slots in the mortuary when there is no room anywhere. With a tired voice, the young doctor said, “There’s nothing we can do…”
April 21
In a television interview with Lithuania’s “Laisvės TV,” Dr. Vaitkus updated some of his earlier information. He noted that autopsy findings of corona patients now show widespread viral sequelae, with microthrombi in the kidneys, heart, lungs, and other organs. On a positive note, two patients have recovered enough to leave the ICU…
April 28
Dr. Vaitkus shared some upsetting news with his family. His mentor and colleague, pulmonologist Dr. JM died from Covid-19 today. “He was always running around, caring for patients.” He was 62 years old and planning to retire at the end of April.
April 30
At the beginning of April, Dr. Vaitkus’ fiancée Dr. Moseley was diagnosed with the coronavirus. She has recovered and is now back to work. She asked her future in-laws for assistance in getting some N-95 masks for herself. But it’s not like she doesn’t have any. She was issued one… 10 days ago.
The interviewer’s reflections
This interview describes the situation of patients admitted to the hospital. Of course, not everyone infected with the coronavirus ends up in a hospital and many people successfully recover. But IMHE experts from Washington, DC, predict that 250,000 U.S. deaths are expected. If we fall ill, we cannot know in advance which group of patients we will fall into. So this is why it is necessary to shelter at home and adhere strictly to all movement restrictions. Let’s not place ourselves or our loved ones at risk. Health care workers work under very difficult and dangerous conditions, and they are doing it for others. Let’s not forget that.
Our collective responsibility can be summed up by a very apt saying I heard recently: a choir can only sing pianissimo if every chorister sings that way.
 DRAUGAS NEWS Lithuanian World Wide News in English
DRAUGAS NEWS Lithuanian World Wide News in English
